Pressure Ulcers/ Injuries
Pressure ulcers are a major burden on healthcare with financial costs of up to 4% of the annual healthcare expenditure in the UK (Bennett. G et al, 2004). Estimated costs for one pressure ulcer per individual are £30,000 (Banks M, 2010). In addition to financial costs the humanitarian costs to patients are many including suffering and pain.
WHAT IS A PRESSURE ULCER/ INJURY?
A pressure ulcer is defined as localised damage to the skin and/or underlying tissue as a result of pressure in combination with shear.pressure injuries usually occur over a bony prominence but may be related to a medical device or other object (epuap/ npiap/ ppia,2019)
Pressure Injury Classification
In order to develop a plan of care for patients with pressure ulcers/injuries it is important for caregivers to understand the extent of tissue damage involved. This can be done by using a classification system which looks at the amount of tissues involed including the skin,subcutaneous fat, bone, muscle,tendon and ligament.
The European pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and the Pan Pacific Pressure Injury Alliance have designed a classification system which allows caregivers to assess the amount of damage involved on visual inspection.
The following descriptions have been taken from the Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline, NPUAP, EPUAP and PPPIA, 2014
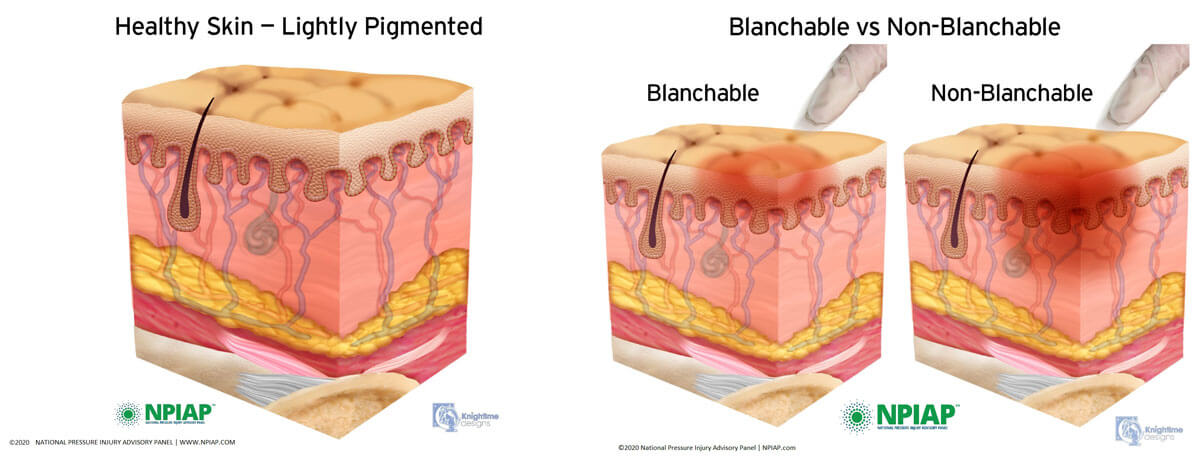
On inspection of the patient’s skin red areas may be observed otherwise known as erythema. It is necessary to establish if the area is a category/stage 1 pressure ulcer/injury. Erythema can be defined as blanching or non-blanching erythema:
Blanching Erythema
When a reddened area is observed on intact skin and finger pressure is applied, otherwise known as the blanch test the area will turn white. This shows that the micro-circulation is intact and the skin is not damaged. It may be a warning that the patient needs to be repositioned to avoid any future damage occurring.
Non-Blanching Erythema
When a reddened area is observed on intact skin and finger pressure is applied the area remains red, indicating that there has been some damage to the microcirculation and a first sign that the skin has the potential to breakdown. This is categorised as a category/stage 1 pressure ulcer/injury.
Nonblanchable Erythema
Partial Thickness Skin Loss
Full Thickness Skin Loss
Full Thickness Tissue Loss
Depth Unknown
Nonblanchable Erythema
Category/Stage I : Nonblanchable Erythema
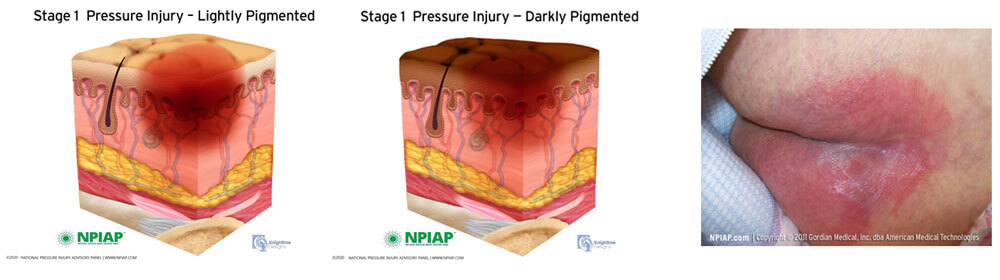
Category/ Stage I pressure ulcer/injury on the buttocks
Description
Intact skin with non-blanchable redness of a localised area usually over a bony prominence. Darkly pigmented skin may not have visible blanching; its colour may differ from the surrounding area. The area may be painful, firm, soft, warmer or cooler as compared to adjacent tissue. Category/Stage I may be difficult to detect in individuals with dark skin tones.Partial Thickness Skin Loss
Category/ Stage II Partial Thickness Skin Loss
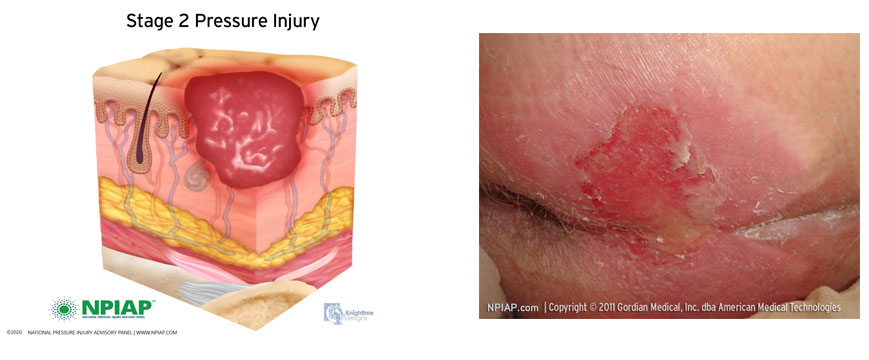
Category/ Stage II pressure ulcer/injury on the buttocks
Description
Partial thickness skin loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough. May present as an intact or open/ruptured serum-filled blister.
Presents as a shiny or dry shallow ulcer without slough or bruising.
Full Thickness Skin Loss
Category/ Stage III : Full Thickness Skin Loss
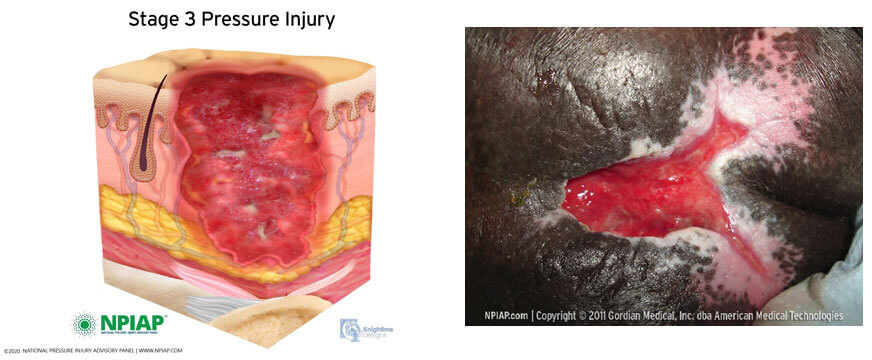
Category/Stage III pressure ulcer/injury sacrococcygeal
Description
Full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon and muscle are not exposed. Slough may be present but does not obscure the depth the depth of tissue loss. May include undermining and tunnelling.
Full Thickness Tissue Loss
Category/ Stage IV: Full Thickness Tissue Loss
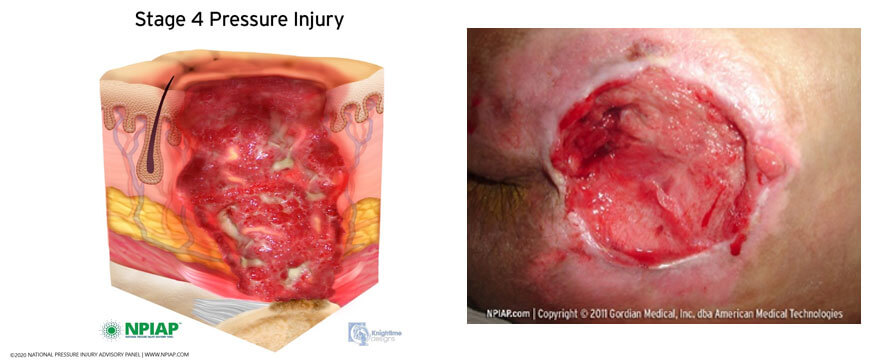
Category/Stage IV pressure ulcer/injury sacrococcygeal
Description
Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound bed. Often include undermining and tunnelling.
Depth Unknown
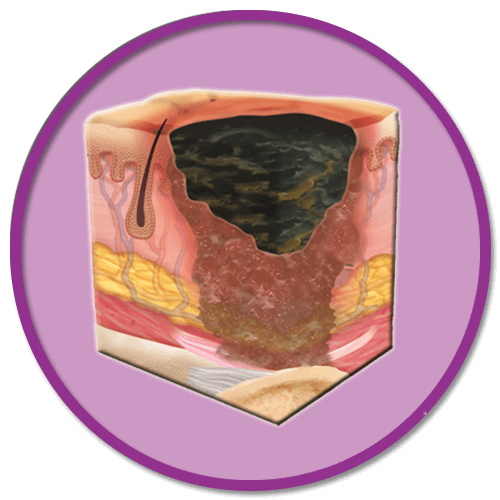
Unstageable: Depth Unknown
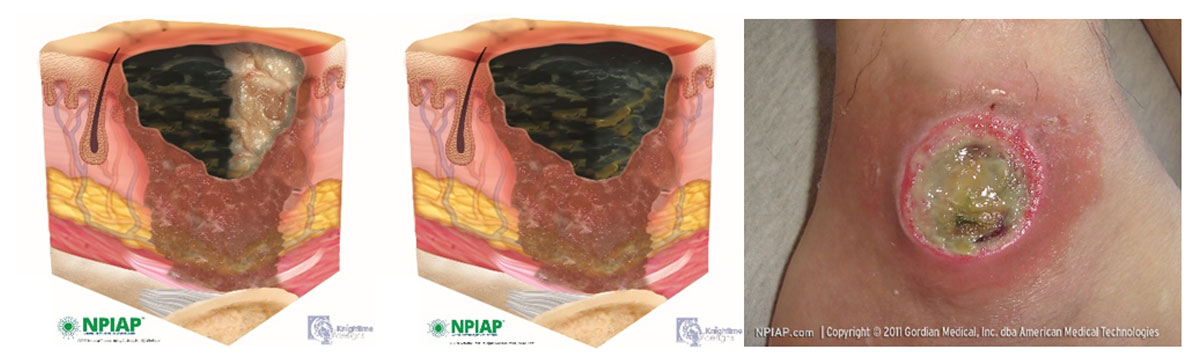
Unstageable: ankle
Description
Full thickness tissue loss in which the base of the ulcer is covered by slough ( yellow, tan, grey, green or brown) and/or eschar ( tan, brown or black) in the wound bed.
Until enough slough and/or eschar is removed to expose the base of the wound, the true depth, and therefore Category/Stage, cannot be determined.
Suspected Deep Tissue injury: Depth Unknown
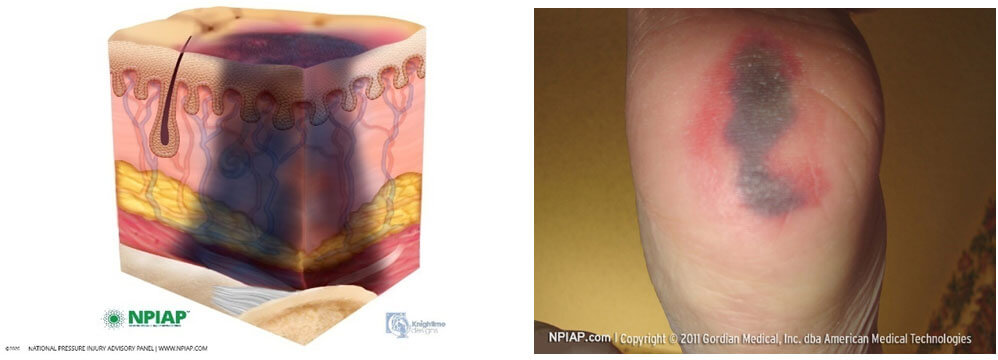
Suspected Deep Tissue Injury: heel
Description
Purple or maroon localised area of discoloured intact skin or blood- filled blister due to damage of underlying soft tissue from pressure and/or shear. The area may be preceded by tissue that is painful, firm, mushy, boggy, warmer or cooler as compared to adjacent tissue. Deep tissue injury may be difficult in individuals with dark skin tones
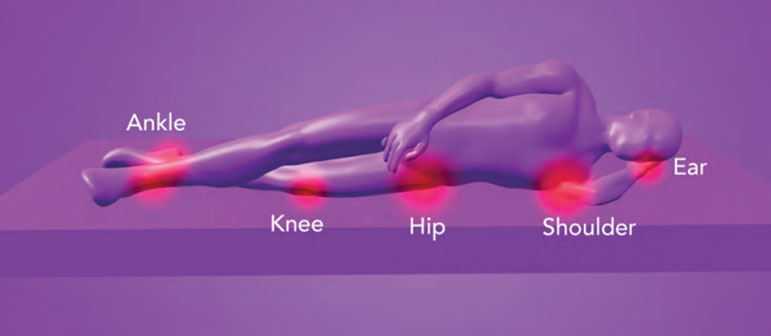
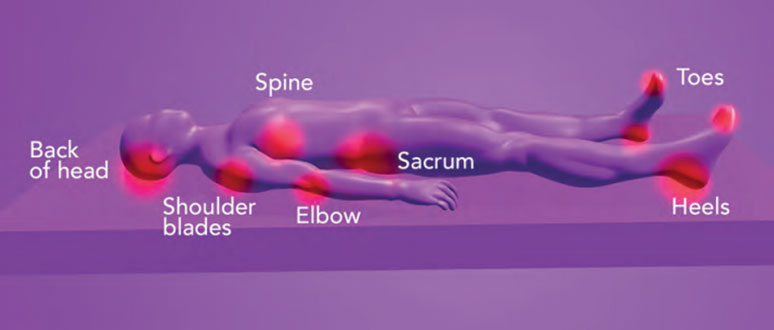
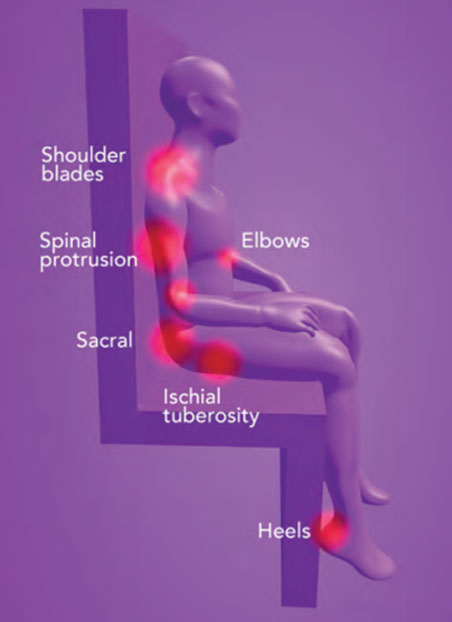
Common sites of Pressure Ulcers/ Injuries
Definition of Tissue Interface Pressure:
Tissue Interface Pressure is the force generated between the body and surface supporting it, meaning that the larger the surface area supporting an individual the lower the tissue interface pressures will become.
Common sites for pressure injuries to occur are in the skin and soft tissues next to bony prominences, where they become compressed between the bony prominence and the surface the individual is lying or sitting on. On a hard surface the pressure points will be higher than those on a softer surface. On a therapeutic surface/mattress which conforms to fit or mold around the body by immersing(sinking) and enveloping /conforming to the shape of the individual, this increases the surface area supporting the individual is increased, maximises weight distribution, reduces tissue interface pressures on the skin and underlying tissues. This is particularly important maintain the microcirculation vital for the maintenance of healthy skin.
Pressure Points
Risk Factors Attributing to Pressure Ulcer/ Injury development
Risk factors
Risk factors which contribute to pressure ulcer/injury development fall into three categories
- – Extrinsic factors
- – Intrinsic factors
- – External factors
These are mechanical forces which cause pressure ulcer/ injuries due to one or as a combination of mechanical forces.
Pressure
![]()
Pressure is a perpendicular force considered to be the main contributing factor to pressure ulcer/injury development. As a result of pressure generated between the body and the support surface supporting it resulting in pressure sufficient to impair blood supply, essential for healthy skin pressure ulcers/ injuries can occur. Pressure is greatest where the skin and soft tissues are compressed between bony prominences and the surface the patient is lying on. Pressure is exerted on the tissues from the downforce of the bone and underlying tissues and the upward force of the supportsurface.
Shear
![]()
Shear is a force which runs parallel to the tissues. It typically occurs when patients slide down beds or chairs due to gravity. Gravitypulls the body down, the skeleton slides down over the surface taking with it the tissue attached to the bone. The skin remains resistant and remains intact with the surface. This action results in distortion and collapse of the capillaries resulting in ischaemia, a reduction in oxygen and nutrients to the skin and potential tissue damage.
The mechanical force of pressure is also always present with shear, a combination of the two can result in greater damage to the skin.
Maturation/Moisture
![]()
When the skin is exposed to moisture which could be due to a high temperature, sweating and incontinencethis could lead to maceration of the skin over time.
Skin damage can occur due to maceration alone and can be diagnosed as a moisture lesion.
Immobility
– The main contributing factor to pressure ulcer/ injury development. The patient is unable to move in response to pain and pressure sensations.
Pain
– Patients in pain can be less reluctant or afraid to move and therefore do not relieve the mechanical forces.
Poor nutrition and hydration
– Without adequate calories, proteins, vitamins, minerals, and hydration this will impact on wound healing.
Neurological Status
– Some diseases cause loss of sensation making them aware of discomfort and the need to reposition themselves.
Body Type
– Being underweight and overweight have their challenges when addressing being at risk of pressure ulcer/injury development. Plus size patients may have difficulty in mobilising and create difficulty for caregivers sometimes resulting in poor moving and handling techniques. Patients who are underweight have less protection with a lack of cushioning over vulnerable areas.
Chronic illness
– The patient with a chronic illness can be at increased risk such as a diabetic who may have a compromised peripheral circulation and lack of sensation.
Medication
– Some medications may have an impact on the patient and their risk of skin breakdown, steroids influence the inflammatory phase of wound healing and give the skin a vulnerable papery thin texture. Strong analgesia may dull the patients senses to change position.
There are other factors which will contribute to pressure ulcers/ injuries which include:
- – Poor fitting clothing and footwear
- – Poor lifting and handling techniques
- – Inappropriate use of equipment
Risk Assessment
When an individual is admitted to a healthcare environment their skin needs to be examined for any damage, they also need to be assessed to determine their risk of developing pressure ulcers/injury.
There are several commonly used risk assessment tools that can be used which have a numerical value associated with the risk of the patient of developing a pressure ulcer/injury. By adding the values will equal a value and as such an indicator to a caregiver what risk category the individual falls into and allows for a plan of care to be created.
Patients should be reassessed after a surgical or interventional procedure, or after a change in their care environment following a transfer (NICE Quality statement 3, 2015)
There are a variety of risk assessment tools:
Whilst a risk assessment tool is an indicator of an individuals identification of risk of developing tissue damage or existing damage it is imperative that this needs additional clinical judgement from the caregiver.
Whilst IQ medical cannot provide advice on all these areas we can pride ourselves on the therapeutic surfaces we provide which support you addressing some of causes of pressure ulcers/injuriesas well as providing comfort and care to your patients
Bennett G et al. The cost of pressure ulcers in the UK. Age and Aging. 2004;33(3): 230-5
Banks M, Graves N, Bauer J, Ash S. The cost arising from pressure ulcers attributable to malnutrition. Clinical Nutrition. 2010;29: 180-6
European Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/ Injuries: Clinical Practice Guideline. The International Guideline. Emily Haesler (Ed.). EPUAP/NPIAP/PPPIA: 2019.
National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Emily Haesler (Ed.), Cambridge Media: Osborne Park, Western Australia; 2014
Quality statement 3: Pressure ulcer risk reassessment | Pressure ulcers | Quality standards | NICE

